On a dreary morning in March 2019, shortly after we lost an hour for daylight savings and my internal clock was thrown for a disastrous loop like it does every half-year, I turned off my three alarm clocks which were completely unnecessary because I hadn't slept a wink, crawled out of bed, and drove over to a ProMetrics testing center near my house to complete the Sports Certified Specialist Physical Therapist exam. I had my photo identification, my registration paperwork, and a list of test day reminders: make sure you remove all jewelry before going through the metal detector, be prepared to pull up your shirt and pants sleeves and have your ears checked, bring water and snacks because your exam is seven hours long but you can have a break in the middle, and a bathroom will be available.

Now, here we are almost the end of June 2019, more than four months later, and today I received the results - I passed my test! I was walking out of basketball practice with the Storm when I glanced at my phone and saw the email with this report. Without the Storm, I would not have met the criteria to even take this exam, because you need sideline coverage hours in a contact sport, and lots of them. I'm so grateful for them. Per the rules of the examination and ProMetrics, I won't go into any details on the actual content of this test, but I wanted to discuss the preparations I used and what advanced certification as a physical therapist even means. Fortunately, I wrote many of these thoughts in March, because there's no way I would have remembered them now! But I couldn't get myself to share it, in case I hadn't actually passed the test!
What does it mean to be a Board Certified Physical Therapist? Right now, if you go to PT school in the USA, you're going to graduate as a DPT - Doctor of Physical Therapy - but you are a generalist. You've learned the basics of physical therapy for all the areas of specialty that a physical therapist can work in and you took a big, terrible test that shows you are competent to practice physical therapy. That test would cover all the different areas of practice and is very broad, covering a lot of topics. After graduation, a new grad physical therapist will get a job and, with or without intention - begin to specialize. To some extent, your job may dictate your specialty because that's the area of practice you're going to focus learning about moving forward. The beauty of this is that you're able to change the area of specialty by working in different settings and pursuing alternative continuing education, but it also means that when we first come out of school - or if we change work settings - we're not very experienced in that care area early on.
When I first graduated, I worked at an adult orthopedic clinic while picking up shifts in a skilled nursing facility. I focused my learning on orthopedics because it was my interest, but I had to learn the basics of the rehabilitation center because the needs of those patients were different. Another example - if you came into the rehab gym at Seattle Children's where I work, you would see physical therapists working with children who have developmental conditions, which looks entirely different from what the sports physical therapists, like me are doing. We're working side by side, all physical therapists, doing entirely different things from the same generalist education. I'm in awe of their work every day... and it's so different!
In some ways, the pathway of a physical therapist mirrors how a physician (MD) completes their schooling. Any doctor you have seen - your primary care or specialist - went to medical school and graduated as a generalist. However they can't practice medicine that way. They are required to continue on their education pathway into a residency, determined by an intense matching program that I'm incredibly thankful I did not have to endure. They will be matched into the field they will pursue and specialize in, like emergency medicine, cardiology, orthopedics, family medicine... that list is super long. And then, after another several years of working in their specialty while learning on the job, they become a specialized physician and can practice in their field. But they don't have the wiggle room to wake up in the morning and say - I don't like being a heart doctor anymore, so I'm going to study diabetes and be a doctor for that. They're a bit more restricted in their careers.
I have read articles recommending that physical therapy transition into the medical school model, requiring residencies to specialize. This is an option now, but it is not required. A physical therapist currently has the option to specialize in nine different areas, and this can be done by either completing a residency program and taking a big test, or by meeting a list of requirements and taking the same big test. This is the test I took earlier this year and have been tortured into waiting four months to get my results. The residency program is meant to give you the hands-on experience and focused training needed to pass the test, but you're able to test without the residency and achieve the same end-goal if you meet specified criteria.
In early 2014 I had applied for residencies in Sports Physical Therapy. I wanted to work in sports and having had years of experience working with women's basketball and a shortage of physical therapists working with the WNBA, I felt this was the direction I needed to go in. At the time, I think there were fifteen programs, but only three had options that were not soccer (none had options specific to women's sports) - and those were the programs I decided to apply to. (No offense soccer, but I'm a fair weather sports girl. I'll support the USWNT all day long and cheer and attend games when the sun is shining, but a year of sideline coverage in the rain was NOT on my To-Do list.) And so - I applied to University of Southern California, Ohio State University, and Duke University. (It would have killed my Husky Heart to be a Blue Devil a little bit, though the education would have been superb at all three institutions). Needless to say, I was not selected for one of the few slots available, a very sad failure, but a few months later I managed to secure a spot in the WNBA without it, so I took the alternative route.
The options for physical therapist
specialist certification right now are: Cardiovascular/Pulmonary, Clinical Electrophysiology, Geriatrics, Neurology, Oncology, Orthopaedics, Pediatrics, Sports, Wound Management, and Women's Health. The list of accredited residency programs is
here for all the specialties. A recent presentation I watched discussed focus on making a new specialty for Pain, which has not yet been established, but that seems like an interesting approach to try to advance the use of physical therapists in treating people with persisting pain. Since I've previously written about pain on many occasions, and I work with the Seattle Children's Chronic Pain Team, I'm excited to see if that will be specialty number ten.
A little about preparing for the exam:
The application deadline for the Sports specialty was July 31, 2018 to test in March 2019. These dates have been consistent annually with all the specialties having application deadlines sometime in July the previous year for a March test date.
That means that if you want to take the test in 2020, you have 1 month to apply - or even less! The application process is pretty complicated for some of the specialties if you haven't completed a residency, so I advise you check it out soon. All the information you could ever need is right
here.
So, once you've applied, the American Board of Physical Therapy Specialties (ABPTS) reviews your qualifications to determine if you're eligible to take the test in your requested area. That takes about 6 weeks. I started studying when I applied, but I know others waited to make sure they could even take their exam. Here's a look at how I prepared.
First, I gathered a bunch of materials to help me determine what content I needed to study.
The materials I used were:
1) The SCS Prep Course from
MedBridge Education which has a nice table of contents covering all the content areas on the exam. They have prep programs specific to many of the specialty areas.
2) I googled "SCS Residency Program Curriculum" on Google. There are many, but I used
this one which outlined a lot of the content topics.
3) I purchased "PT Sports Questions" by Matthew P. Brancaleone PT, DPT, SCS AT, CSCS" a question/answer
book off Amazon for $35.
4) I already have my CSCS (Certified Strength and Conditioning Specialist) and the
book "Essentials of Strength Training and Conditioning" and the study guide I made when preparing for that test.
5) I borrowed "The Fundamentals of Athletic Training"
book from my boss

6) I found my course materials from the Emergency Management Course I took at REI which was a required pre-requisite to take the exam.
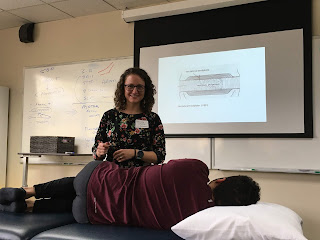
7) I borrowed the Manual of Structural Kinesiology from the Seattle Children's Inter Library Loan System for a review of anatomy and biomechanics basics, particularly with regard to the mechanics of the shoulder, and review of throwing motions and gait cycle. My test was two weeks before giving
this presentation at Seattle Children's so I was preparing for both at the same time.
8) Per the recommendations of the curriculum in #2, I secured copies of the National Athletic Training Association Position Statements, all of which are free
here as well as many of their consensus statements and several of the APTA Clinical Practice Guidelines
here. The highlight of reading those was seeing how many of my UConn mentors were authors of them, including Lindsay DiStefano, Doug Casa, and Robert Huggins. Man UConn puts out some amazing stuff!
9) Lastly, and probably most importantly, the
Description of Specialty Practice (DSP) for my exam. The APTA has a breakdown for each exam listing the material that would be covered on it. If you're approved to take the test, they send it to you as part of your application fee. Or you can buy it before you apply.
Second, I took a practice test. Right from the start. The MedBridge Prep Course offered several practice exams that were shorter in duration than the actual test and covered a wide variety of topics. Based on the results of my first practice test, where some of my outcomes were abysmal, I knew how to prioritize things.
Third, with my current skills clearly identified, and more importantly, my biggest weaknesses, I looked at this ginormous pile of stuff to read and the ~80 hours of online MedBridge videos available, and, I made a study schedule. This is the same approach I took when studying for the PT licensing exam, so I was optimistic it could be successful again. I tried to cluster things together in a sensible way. For example, when I read the chapter in the Athletic Training book about weather-related injuries like heat stroke or how to deal with lightning, I also read the NATA position statements related to the chapter, and then watched the Medbridge Video on that same topic.While I was studying the weather-related injuries, two quotes stuck out to me that I had saved for this post With regard to cold-related illness: "Nobody is dead until they are warm and dead." So, if you find someone buried in the snow, they're not dead until their body has been warmed up. And with regard to lightning injuries, "In the contest between people and lightning, lightning always wins." So I got the repetitions for a topics and kept notes on things that I was unfamiliar with or wanted to come back to after I had gone through everything once. Repetition is helpful for me, but also sometimes felt like I was beating a dead horse by the end of some of the longer (or less interesting) topics.
And then I took my test. I'll be honest - I was behind on my schedule pretty much from the second week, but I just kept plugging along. I had an excellent student in the clinic, who I wrote about
here and
here, and who was treating about half of my case load for several weeks leading up to the test, allowing me more time to devote to reading papers and studying. I read A LOT of the materials listed above, but found some of it to be too inapplicable to the patient care I typically do, that I decided it was worth leaving out some chapters despite the risk of doing so. I watched almost every single Medbridge course that was listed in their prep program, several just listening while I was driving, including most of the optional ones. I was stuck on the Brooklyn Bridge for over an hour in traffic and watched an entire course on nutrition in that time. And I was certain that I did not pass. Today's news that I passed was super exciting. Hopefully writing up my preparations will help someone else on their road to board certification.