|
| with permission from the Level Up Initiative |
 |
| Zak Gabor with me in 2017 |
The Level Up Initiative strives to educate physical therapists (and other healthcare providers) on a biopsychosocial approach to patient care focusing on soft skills and therapeutic alliance in addition to the anatomical tissue healing factors and movement patterns we learn in school. The goal is to teach clinicians ways to interact with their patients with critical thinking, to connect, to prioritize using positive language and a growth mindset, and to focus less on a medical diagnosis and more on the whole person. Increased consideration for mental health and psychology, far more than what I learned in PT School is a factor of the paradigm shift. My school taught the biomedical model with primary consideration of anatomy and biomechanics without much attention to the psyche or nutrition or sleep or a whole host of other stressors that impact our patients. Most schools are just like this, though as the shift continues, more programs are giving attention to these considerations.
 |
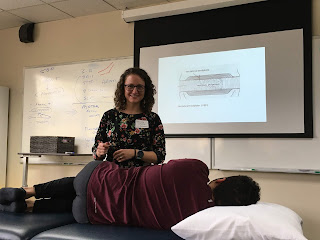
| Ellie leading our Mentorship Group |
The mentorship program lasts four months and, as already mentioned, is free. Free! These skills will immediately impact your patient care, but you have to put in the effort to go through their materials. They send you the full course syllabus in advance which outlines the recommended books, podcast episodes, TED talks, and publications to go through over the program and you can really dive in at your own pace. The course is organized with themes that help to focus the group discussions, but going out-of-order with the reading didn't impact my experience. I chose to complete all the tasks on the syllabus, but I could see that if your schedule didn't allow for that, you could take it as a reading list to work through in the future while still getting a lot out of the discussions and watching the modules.
I won't tell too many details about the specific resources because you should participate in it to get the full experience, but I do want to share some of my favorite parts and describe the structure hoping that it will encourage you to sign up for their next cohort (HERE). The three key topics explored in the mentorship program are Growth Mindset, Critical Thinking, and Communication. Even as a PT for the past five years, I learned new things with each topic, and regularly wished I could have had this knowledge as a new grad. Each topic had discussions amongst our assigned mentorship group as well as reflection questions to consider for personal growth.
 |
| Photo from Module 1 with permission from Level Up |
Module 2 dove into Critical Thinking. If we want to see change across PT and across healthcare, we have to start changing how we practice so that the field can catch up to our individual change. We need to challenge the things we learn in school and we need to challenge our own thought processes in order to grow. Critical Thinking is an umbrella term that really encompasses many concepts - including an open mindset (like module 1) and communication (the next two modules), but for me, the biggest part of critical thinking is to recognize our own biases and look for ways to disprove our own opinions and beliefs. When I took Greg Lehman's "Reconciling Pain Science with Biomechanics" Class which I wrote about last week here, I asked him how he organized his learning because he reads SO MANY articles. He told me that he will pick a topic and then collect several resources on that same topic looking for ways that his beliefs can be changed while reading the collection. That is intentional critical thinking.
 |
| with Permission from the Level Up Initiative |
One of the recommended books for this topic was the toughest book I've read since "Explain Pain Supercharged," but once I got past the big words I needed to learn, I was really impressed by the brilliance of the book and by the importance of the concepts outlined in it. Where does vulnerability fit into our careers as heathcare providers? How much can we tolerate uncertainty? We need to reflect on the care we provide so that we can identify our personal areas with room for growth. We also need to recognize that our interactions with our patients are directly impacted by our own beliefs and the patient's beliefs. The motivation of a patient will impact their participation in your home exercise program. If it looks relevant to an activity they strongly want to return to, that's different than if your recommendations seem arbitrary and unable to help them achieve their goals. If I believe that jumping up and down is going to help my patients and I can convince them to do it with intelligent rationale of how it will help them return to running, they're going to do it. If my coworker uses a different approach, they're going to use an alternative treatment technique. Potentially neither of us wrong, but if the patient thinks my way is better, it will impact their care. Because of this, earning a patient's trust can really outweigh other things in care. Remember, we're not treating robots. To focus entirely on the objective and ignore what the patient thinks is going on with their own body, aka the subjective, leaves holes in their story and makes it harder for you to effectively treat patients.
So after four months and lots of new learning, I'm excited to share about the experience with you, and hope that if you're a new graduate PT, you'll consider participating in this mentorship program in the future. Sign up this week, or wait until the next round. Follow the Level Up Initiative on their social media sites, all linked above. And then let me know what you think. Tell them I sent you.